Research questions ‘iron deficiency’ as key cause of anaemia in India
Research questions ‘iron deficiency’ as key cause of anaemia in India
The conventional wisdom, that iron deficiency is the primary cause of anaemia in India, may be outdated, with a host of other factors, ranging from a Vitamin B12 deficiency to air pollution, influencing anaemia, says a study involving researchers from multiple institutions that was published earlier this week. Moreover, the manner in which blood is drawn for testing anaemia in public health programmes can dramatically alter estimates of the condition.
The study has appeared in the peer-reviewed European Journal of Clinical Nutrition.
Anaemia, characterised by weakness and fatigue, and paleness among other symptoms, is due to a lack of enough red blood cells (RBC) or haemoglobin, the carriers of oxygen to cells. The common wisdom is that insufficient iron – necessary for the liver to produce RBC – is the culprit and is the driving force behind public policy interventions such as iron supplementation or mixing iron into staple foods (bio-fortification).
The latest official assessment of anaemia in the fifth round of the National Family Health Survey (NFHS), in 2019-2021, suggests that despite decades of policy intervention, anaemia had only gotten worse. The prevalence in India had risen from 53.2% to 57.2% in women of reproductive age, and from 58.6% to 67.1% in children, compared to the previous NFHS-4 conducted in 2015–2016.
The latest study, funded by the Department of Biotechnology, measured venous blood haemoglobin (Hb) concentrations from about 4,500 people in eight States. Overall, 34.9% of those tested were anaemic. However, only 9% of them had what could be medically characterised as iron-deficiency anaemia; 22% of them were characterised as having anaemia from ‘unknown’ causes.
“The major proportion of anaemia in all groups studied, was due to… unknown (and unmeasured) causes of anaemia. This could be due to deficiencies in other erythropoietic (blood-producing) nutrients like B12 or folate, or due to hemoglobinopathies, undetected blood loss, an unhygienic environment [20] or other causes like air pollution,” the authors said in their report. The team of scientists and doctors spanned institutions such as St. John’s Medical College, Bengaluru; the National Institute of Nutrition (ICMR), Centre for Cellular and Molecular Biology, and Institute of Genomics and Integrative Biology, among others.
For women aged between 15 and 49, anaemia prevalence in the eight States was 41.1% in comparison with 60.8% in the NFHS-5. The prevalence of anaemia in adolescent girls (15-19 years) – as a group that is the most anaemic – in the eight States was 44.3% compared to 62.6% in NFHS-5. The same trend persisted in adult men (20.7% vs 26.0%) and adolescent boys (24.3% vs 31.8%) between the comparable age groups in NFHS-5. Assam had a very high prevalence of anaemia (between 50%-60%) and relatively low iron deficiency (18%), suggesting that other factors may be responsible.
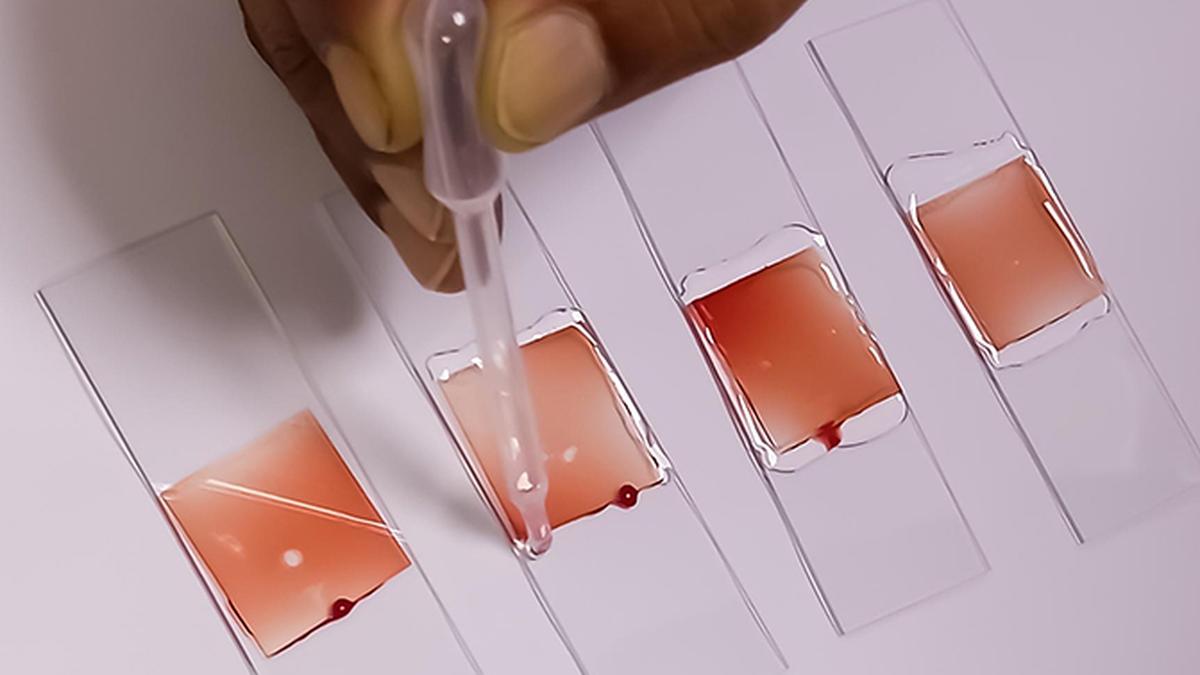
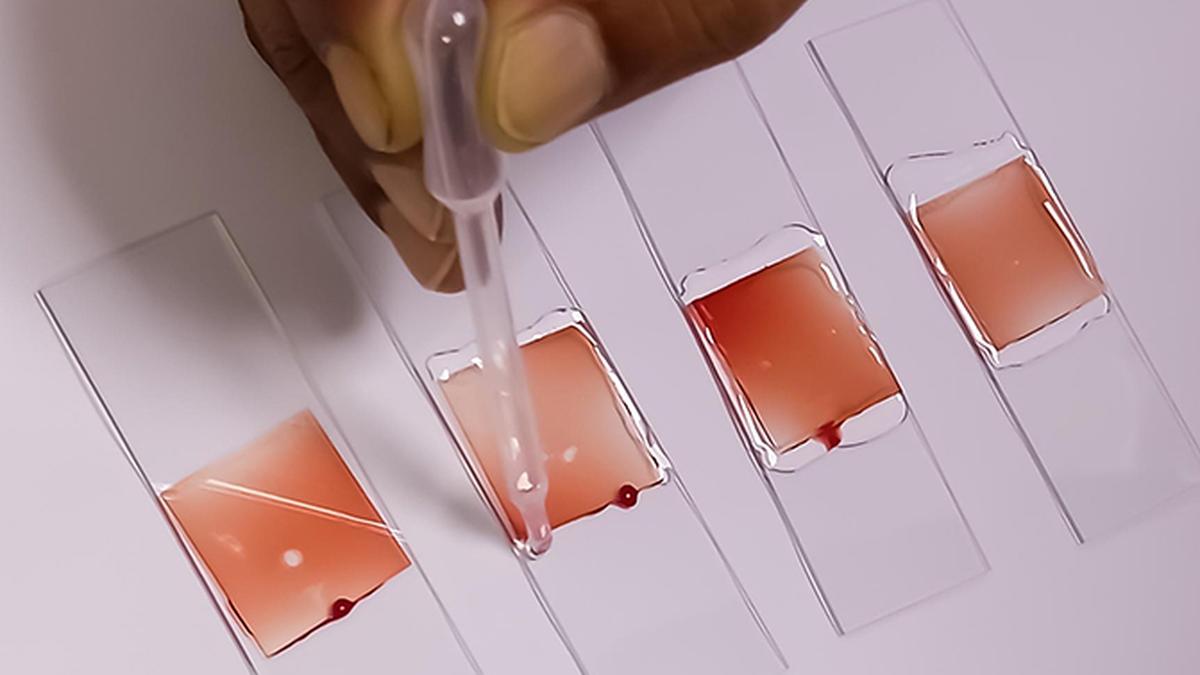
The percentage drop in anaemia in this study compared to the NFHS could be explained by the method of blood collection, said Anura Kurpad, professor, St. John’s Medical College, and one of the authors of the study. The NFHS relied on drawing capillary blood, or from a pinprick, compared to the more involved venous-blood draw. Because NFHS relied on district-level collection, the former method was preferred because of logistics and cost. Capillary blood was blood drawn from the tissues and “mixed” with other body fluids, possibly influencing the estimation of Hb. Since last year, the World Health Organisation had recommended that venous blood be the recommended method for estimating anaemia.
That iron deficiency was responsible for only a minority of anaemia prevalence suggested that it was time for a more nuanced policy intervention to address anaemia.
Dr. Kurpad said that the results of the study pointed that concentrating on single interventions, such as iron tablets or folate acid on their own, was inadequate. “The key is to diversify diets. We have to intervene with ensuring more fruits, milk and vegetables are made available to a wider population which will improve absorption of essential nutrients. We have to change the economics to make high quality diets and not just single nutrients, more accessible,” he told The Hindu.
To address anaemia, the Centre has an Anaemia Mukt Bharat (Anaemia-free India) initiative with six interventions – prophylactic iron folic acid supplementation; periodic de-worming; intensified year-round behaviour change communication campaign; testing of anaemia using digital invasive haemoglobinometer and point of care treatment; mandatory provision of iron folic acid fortified foods in public health programmes.